Stress, IBS and the Gut-Brain Axis
-
What's the connection between our bowels and our brain?
-
Benjamin Brown explains how to improve IBS symptoms by managing stress
-
Therapy can help with stress - you can find a therapist here
Stress plays a major role in the development of digestive problems. Stressful events alone can trigger symptoms, such as pain and diarrhoea, and if you are chronically stressed symptoms tend to be more severe. About 75 per cent of people with IBS report having serious stress-related symptoms, such as anxiety and depression, and while having digestive issues is itself very stressful, there is good reason to believe that stress can be one of the reasons why you develop symptoms in the first place.
Trauma in early childhood such as conflict in the family, severe illness, the death of a close family member and mental or physical abuse has been shown to predispose children to the development of IBS later in life. And more recent life stress may play a role as well. In a survey of about 1000 adults without IBS, it was found that people who had anxiety and depression were far more likely to develop IBS.
In one study, chronic life stress was found to affect the majority of people with IBS and, in fact, appeared to be the main reason why their symptoms got worse. So how exactly does stress affect your digestive system?
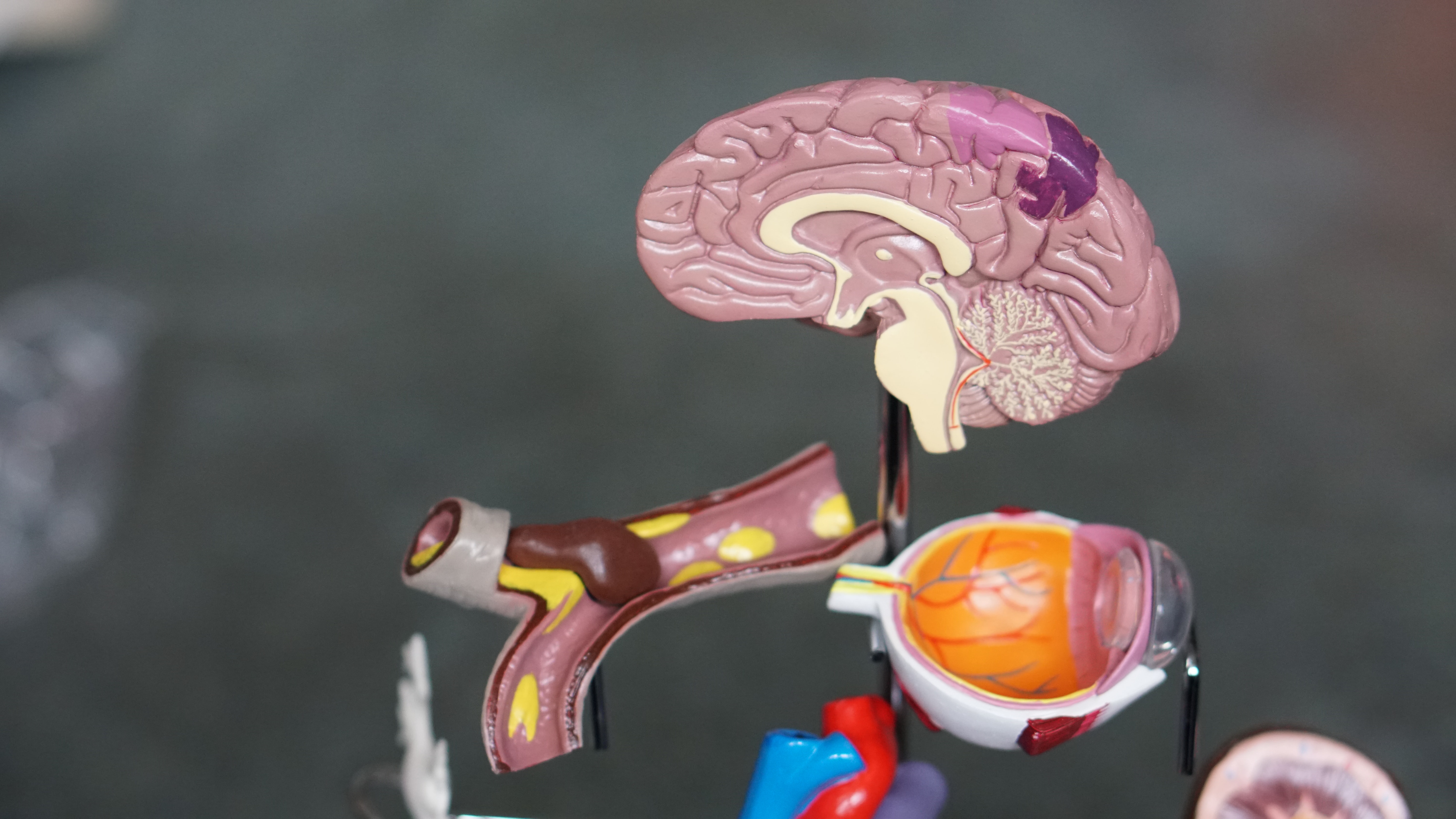
The gut-brain axis
When you face a source of stress your brain reacts by producing hormones that travel throughout your body to help you adapt to the situation. This includes increasing your mental alertness and increasing oxygen and blood flow to the brain and muscles in what is known as the ‘fight-or-flight response’. In our ancient past this response was important for dealing with short-lived threats or challenges to our survival, however in the modern world the stressors we face are more likely to be daily worries and emotional stress. So your brain and nervous system are under constant pressure which also means your stress hormones can be travelling around your body at unusually high levels for long periods of time.
If you have ever felt chronic fatigue, worry, anxiety or simply unable to cope, there is a good chance you have suffered from chronic stress, as these are some of the most common symptoms. What you may not be aware of is just how dangerous the effects of chronic stress are. It can lead to an endless array of health problems including anxiety disorders, major depression, insomnia, infections, allergies, autoimmune disease, diabetes, weight gain, heart disease, chronic fatigue syndrome and, of course, digestive problems.
Your brain and digestive system are in constant communication via what is referred to as the gut-brain axis. Your brain through various hormones and nerve pathways controls normal digestive function. Stress hormones, such as cortisol and adrenaline, can influence your digestive function via the nerves that travel directly from your brain to your gut. This communication superhighway travels both ways, which means that digestive problems can affect your mood and behaviour too.
The stress of living with digestive illness
Living with digestive symptoms can be a traumatic experience. Pain and other symptoms can provoke anxiety, depression and mental exhaustion. Diarrhoea or a sense of urgency, for example, can cause extreme worry because of the possibility of not making it to the bathroom on time. Bloating and distension can be unsightly and embarrassing, and constant pain can have a tremendous impact on mental health and wellbeing.
Coping with symptoms can be very difficult and a fear of symptoms can stop people from engaging in social activities. Family and social relationships are frequently affected, as can be marriages and sexual relationships.
People can be afraid to eat at work for fear of symptoms and may withdraw socially causing further anxiety, anger, guilt and shame. Your mind, gut, emotions and experiences all interconnect to create important intertwined relationships that need to be considered if you are going to improve your symptoms. This understanding of how emotions influence digestive symptoms and how digestive symptoms can conversely influence emotions via the gut–brain axis is central to how mind-body therapies can improve your physical and emotional health.
What can you do to reduce the stress of IBS?
1. Manage your stress levels
You can do this by seeking immediate relief from natural medicines, such as peppermint oil, artichoke leaf extract or aloe vera juice, and by embracing long term stress management tools such as abdominal breathing exercises and meditation. Because our symptoms are inextricably linked to your mental and emotional health, basic stress management strategies are important for your recovery.
2. Try cognitive behavioural therapy
Cognitive behavioural therapy (CBT) is the best-studied mind–body therapy for IBS and has been shown to be effective for improving gastrointestinal symptoms and psychological distress. CBT works by progressively changing behaviours that perpetuate symptoms while instilling new adaptive behaviours, such as relaxation or meditation, to effectively manage the illness. Typically, a trained therapist facilitates CBT over ten to twelve sessions.
3. Try hypnotherapy
Specially developed gut-focused hypnotherapy has been shown in a number of studies to improve gastrointestinal symptoms by about 50 per cent by reducing psychological symptoms and improving general life functioning. Most people seem to respond well and benefits appear to be maintained for some years afterwards. The treatment involves a practitioner inducing you into a hypnotic state of deep relaxation and then guiding you through therapeutic suggestions, including muscle relaxation, further relaxation of your gastrointestinal system and strengthening your inner resilience, through visualisation.
4. Try other mind-body therapies
A number of mind-body therapies have been investigated including psychodynamic psychotherapy, biofeedback therapy, progressive muscle relaxation, yoga, meditation, mindfulness, relaxation and stress management. All these have shown some indication of benefit, in particular psychodynamic psychotherapy. If a particular mind-body therapy appeals to you it is worth seeing if regular practise or treatment helps.










